Viral Knowledge
Researchers Investigate How Flu and Colds Spread, and How to Predict Them
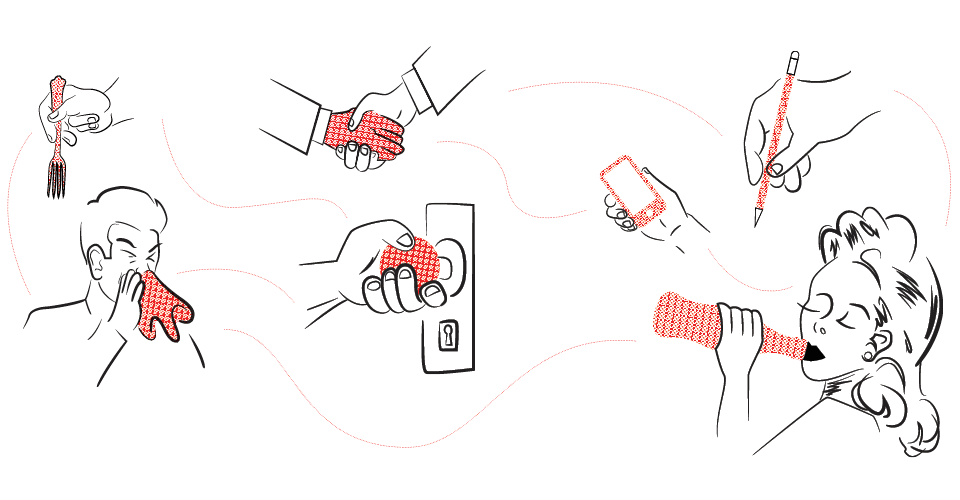
by Chris Carroll | Illustration by Jason KeislingIt’s almost 70 degrees on a pleasant spring day, but in a lab at the School of Public Health, Maria Pozo ’19 huddles in a sweater and puffy vest and hacks out a percussive series of coughs.
The bioengineering major has no idea how she fell ill—no one she knows is obviously sick, and she doesn’t recall being blasted recently by a stranger’s random sneeze.
The fact that health science itself is almost equally mystified explains why Pozo is about to spend half an hour with her face stuck in a trumpet-like metal tube. It’s attached to filters, tanks and other gadgetry that will vacuum up virtually everything that comes out of her lungs for further study.
“Believe it or not, how people transmit flu and other respiratory illnesses is not understood,” says Don Milton, a professor of environmental and occupational health, who invented the so-called “Gesundheit machine” and is now running the unique study in which Pozo is participating.
He, a team of faculty investigators and students have been tracking hundreds of undergraduates around campus, observing when and how they get sick, summoning their contacts and testing them as well, measuring ventilation in their rooms, even testing the germs on students’ ever-present cell phones.
The monitoring began in spring 2017, targeting volunteers from a group of about 150 students enrolled in College Park Scholars’ Global Public Health Scholars program or their roommates in Centreville Hall. The program was extended this school year to students in the Science, Technology and Society and Life Sciences programs as well.
The primary research aim of the project, supported by the U.S. military’s Defense Advanced Research Projects Agency (DARPA), is to locate biomarkers in blood—genes that have been switched on in reaction to infection, for instance, or the presence of certain proteins—that will reveal if someone is about to become contagious.
Such predictive ability would revolutionize the ability to control outbreaks of scary, emerging respiratory diseases like sars, says Col. Matt Hepburn, a U.S. Army doctor who manages DARPA’s infectious diseases research portfolio. Contacts of initial disease carriers could be precisely targeted for treatment with potentially scarce supplies of medication, or possibly quarantined.
“Now we have to wait for people to get sick, and by then they might have infected others, so the outbreak spreads and spreads,” Hepburn says.
While collecting the biological samples for DARPA’s biomarker venture, Milton and his team are also delving into every aspect of person-to-person transmission of colds and flu—like measuring how much virus individuals eject into the air around them or onto surfaces, or how dorm room ventilation influences contagiousness or if stress and health habits play a role in illness susceptibility.
“If for example we could show influenza is airborne… and we know how much virus people shed into the air, we could design buildings with ventilation designed so that you don’t transmit influenza,” Milton says.
Observation of students passing germs around is likely the first study of its kind, Hepburn says—feasible only because of the confluence of a world-class influenza transmission expert with a group of long-term, willing study participants right across the street.
“It’s a unique setup, and I think there are few places in the world that would be able to pull this off,” he says.
Just how willing Milton’s subjects are is illustrated by biology major Jillian Macchia ’20, who went in for a series of blood draws and sessions breathing into the Gesundheit machine in early April. She admits she was moderately pleased to have contracted the cough that allowed her to directly participate.
“This is a really interesting study, so I guess getting to be part of it makes getting sick a little nicer than it would be otherwise,” she says.
0 Comments
Leave a Reply
* indicates a required field